
It begins with an itch. That familiar irritating feeling, swiftly followed by the inevitable scratch. For most of us it ends here, in a fleeting moment of bliss. But then there are those tortured few for whom scratching provides little relief.
In 1660, the German physician Samuel Hafenreffer defined an itch as “an unpleasant sensation associated with the desire to scratch.” As an operational definition, it does the job. As far as we know, every animal with a backbone has a scratching reflex. It’s a useful instinct to rid yourself of fleas, mites, mosquitoes and other small insects that might carry infection. But this protective mechanism can also go awry.
In a masterful essay entitled The Itch, the surgeon Atul Gawande recounts the case of an HIV patient suffering from a severe chronic itch. The patient had recently been diagnosed with shingles, a disease whose symptoms often include extreme itchiness. After many sleepless nights of relentless scratching, she woke up one morning with a greenish fluid trickling down her face. Hours later, in the emergency room, her doctors informed her that she had managed to scratch through her skull, all the way to her brain.
Chronic itching is triggered by various diseases, such as eczema, shingles, HIV, chronic kidney problems, or even as a side effect from some medications. In most cases, it adversely affects quality of life, as patients are constantly tortured by their incessant need to scratch themselves. Standard medications often have no effect. These are people who are suffering from an itch that they can’t get rid of.

The story of itch is inextricably woven with the story of pain. Starting from the discovery of morphine in the early 1800s, there has been steady progress in the medical understanding of pain. Researchers have mapped the circuitry that transmits pain, and have developed increasingly effective painkillers and anaesthetics. In contrast, an itch was not considered life threatening, and relatively little effort was spent trying to understand it. For a long time, it was simply thought to be a dull form of pain.
But this picture is changing fast. In the last decade, researchers have learned about receptors in the nerves under our skin that react specifically to itchy substances. When these receptors fire, they send a signal racing up our spinal cord, headed to our brain where it creates an urge to scratch. Scientists now have a basic map of the roads that an itch takes on its way to our brain. And they have even been able to block some of these roads in mice, essentially preventing them from feeling an itch.

There are broadly two types of chronic itches. In the first type, mast cells under the skin release a chemical called histamine. Nerve cells have receptors that ‘sniff out’ the presence of this histamine, and trigger an itch reaction. Many of us who suffer from seasonal allergies have to take antihistamine drugs to block our over-reacting histamine receptors.
But most chronic itches do not respond to antihistamine. For example, chloroquine is a drug that has been used to treat malaria since the 1940s, although it has an adverse side effect in dark-skinned Africans. In some African countries, 70 percent of patients treated with chloroquine develop an itch. It can become serious enough that many are forced to discontinue the medication. In Africa and India, there’s an infamous bean plant called cowhage. The local population of Northern Mozambique call it the ‘mad bean’, because those who touch it to begin scratching vigorously and uncontrollably. This severe itching reaction is often treated with herbal remedies, such as cow dung in India, or moist tobacco in Mozambique. The itching reactions caused by chloroquine or cowhage don’t respond to anti-histamines. Certain opioids used to treat pain, such as morphine, can also cause a histamine-independent itch as a side effect.

Researchers are now learning how these itches develop. In 2007, a study by Yan-Gang Sun and Zhou-Feng Chen studied a receptor called GRPR (gastrin releasing peptide receptor) present in certain nerve cells in the spinal chord. The researchers compared mice that have a functioning GRPR receptor to genetically modified mice that lacked the receptor. After a series of standard pain perception tests (involving prodding these mice with heat rays, and putting them on hotplates), they learned that the mice lacking the receptor were no different from normal mice in their sensitivity to pain.
Next, they injected these mice with different itch causing compounds. Some of these were histamine mediated, whereas others, such as chloroquine, were not. What they found is that in all cases the mice lacking the receptor would scratch themselves less than the normal mice. In a follow up study in 2009, they specifically destroyed the nerve cells in mice that carry this GRPR receptor. These new mice were still just as sensitive to pain, but would barely scratch themselves when injected with a host of itch causing compounds. By removing the GRPR receptor, the researchers had effectively closed the door to itch, while pain could still reach the brain through a different door.
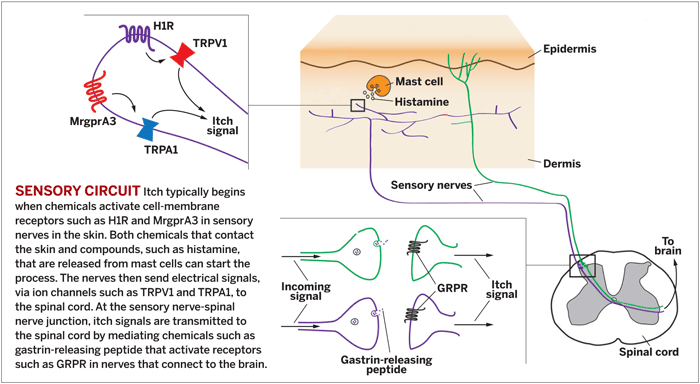
The picture that is emerging is a complex one, where pain and itch signals are distinct yet subtly intertwined. Of the nerve cells under our skin, some are involved only in signalling pain, and they have pain receptors. Others are responsible for signalling different types of itches, and they have both itch and pain receptors. If the same cell has both receptors, how do we distinguish itch from ouch?
The answer is still unclear. A recent study published this April dissected the mechanism by which the malaria drug chloroquine creates an itch. The drug is first detected by an itch receptor on nerve cells. This then activates a pain receptor called TRPA1, the same receptor that detects the painful, sinus-clearing ingredient in wasabi and spicy mustards. Somehow our brain interprets this fiery mix of signals as an itch.
As the biology of itching becomes better understood, the benefits are making their way from the lab to the clinic. The drug morphine is a powerful painkiller, but has a common side effect of itchiness. Women taking opiates to relieve their labour pain often experience a similar side effect. Zhou-Feng Chen and Yan-Gang Sun, authors of the GRPR receptor study, teamed up with colleagues at the newly founded Center for the Study of Itch and managed to tackle this problem. Their results, published in the current issue of the journal Cell, show that the benefits of morphine can be separated from the itch.
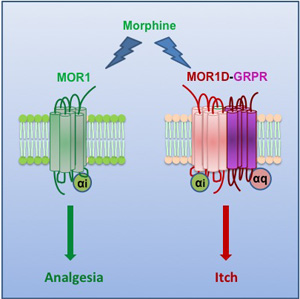
The researchers discovered that morphine acts through two channels. One channel is an opioid receptor called MOR1, which triggers the analgesic effect of morphine. However, we carry another altered form of this receptor, MOR1D, that is also activated by morphine. This other channel triggers the GRPR receptor, resulting in an itch. By blocking this altered receptor in mice, the researchers were able to eliminate the itch, without diminishing the pain-killing effect of morphine.
The science of itch is still in its infancy. Studies in the past decade were focused on mapping the various genes and pathways that mediate itch. The next step for researchers is to develop new drugs that will target these genes in humans. The hope is that we may eventually come up with a scratch to soothe every itch.
References
Sun, Y., & Chen, Z. (2007). A gastrin-releasing peptide receptor mediates the itch sensation in the spinal cord Nature, 448 (7154), 700-703 DOI: 10.1038/nature06029
Sun, Y., Zhao, Z., Meng, X., Yin, J., Liu, X., & Chen, Z. (2009). Cellular Basis of Itch Sensation Science, 325 (5947), 1531-1534 DOI: 10.1126/science.1174868
Wilson SR, Gerhold KA, Bifolck-Fisher A, Liu Q, Patel KN, Dong X, & Bautista DM (2011). TRPA1 is required for histamine-independent, Mas-related G protein-coupled receptor-mediated itch. Nature neuroscience, 14 (5), 595-602 PMID: 21460831
Liu XY, Liu ZC, Sun YG, Ross M, Kim S, Tsai FF, Li QF, Jeffry J, Kim JY, Loh HH, & Chen ZF (2011). Unidirectional Cross-Activation of GRPR by MOR1D Uncouples Itch and Analgesia Induced by Opioids. Cell, 147 (2), 447-58 PMID: 22000021